Stem Cell Therapy for Heart Disease in Malaysia: 2025 Patient Guide
Estimated Reading Time: 8-9 minutes
Table of Contents
Introduction
Cardiovascular disease (CVD) remains a leading cause of death across Asia. According to the World Health Organization, low- and middle-income countries, many in this region, bear a disproportionate burden, accounting for nearly 50% of global CVD mortality. In particular, ischemic heart disease and stroke continue to drive rising death and disability rates.
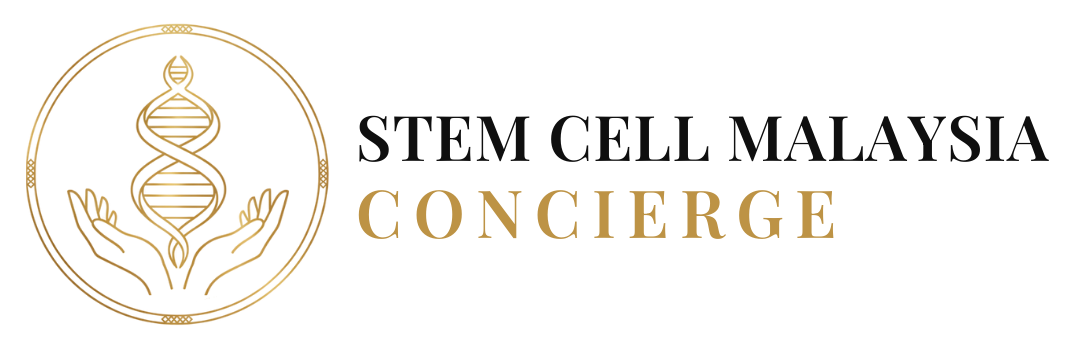
Recent projections in The Lancet Regional Health – Western Pacific warn that this trend will persist through 2050, driven by widespread metabolic risk factors such as high blood pressure, obesity, elevated glucose, and sedentary lifestyles.
As conventional treatments focus on symptom control rather than tissue repair, interest is growing in regenerative therapies, especially stem cell–based approaches. This guide explores the landscape of stem cell therapy for heart disease in Asia, with a particular focus on Malaysia, where private facilities are offering cutting-edge options for both local and international patients.
What Is Heart Disease?
“Heart disease” (or cardiovascular disease) is an umbrella term for disorders affecting the heart and blood vessels. Common types include:
- Coronary Artery Disease (CAD): Narrowing of arteries supplying the heart, often leading to chest pain (angina) or heart attack
- Heart Failure: When the heart is unable to pump enough blood to meet the body’s demands
- Arrhythmias: Abnormal heart rhythms, such as atrial fibrillation
- Cardiomyopathy: Disease of the heart muscle, making it weaker or stiffer
Impact in Asia
Cardiovascular disease is the leading cause of death across Asia. Common manifestations include:
- Myocardial Infarction (Heart Attack): Occurs when blood flow to the heart is blocked, causing permanent damage to heart muscle
- Chronic Heart Failure: Progressive condition where the heart cannot pump efficiently, leading to fluid buildup and fatigue
- Post-Infarction Complications: Scarring and weakened heart function following heart attacks
Regional Trends
Recent epidemiological studies suggest that cardiovascular disease (CVD) in Asia follows unique patterns compared to Western populations.
- The region bears a disproportionately high rate of premature CVD deaths, especially in younger and working-age adults [JACC Asia, 2021]
- Metabolic risk factors such as diabetes, hypertension, and obesity are rising rapidly, driven by economic and nutritional transitions [PMC, 2020]
- Urbanization and lifestyle changes, including sedentary behaviour and unhealthy diets, have become key drivers of CVD burden [Wiley, 2008]
Current Treatment Limitations
Standard treatments include:
- Medications (beta-blockers, ACE inhibitors, statins)
- Surgical interventions (bypass surgery, stenting, pacemakers)
- Lifestyle modifications (diet, exercise, smoking cessation)
Key Limitation: While these approaches manage symptoms and prevent further damage, they cannot regenerate dead heart muscle tissue. Once cardiac cells are lost, they typically do not regenerate naturally, leading to permanent functional impairment.
What Is Stem Cell Therapy for Heart Disease?
Stem cell therapy is a field of regenerative medicine that introduces stem cells or their derivatives into damaged tissues with the goal of repair and restoration. In the context of heart disease, it aims to:
- Regenerate damaged myocardial tissue
- Stimulate new blood vessel formation (angiogenesis)
- Modulate inflammation and scar formation
- Improve cardiac function and reduce symptoms
The most commonly studied cells are mesenchymal stem cells (MSCs), which may be derived from sources like umbilical cord tissue, bone marrow, or adipose tissue.
How Stem Cells May Help: Mechanisms of Action
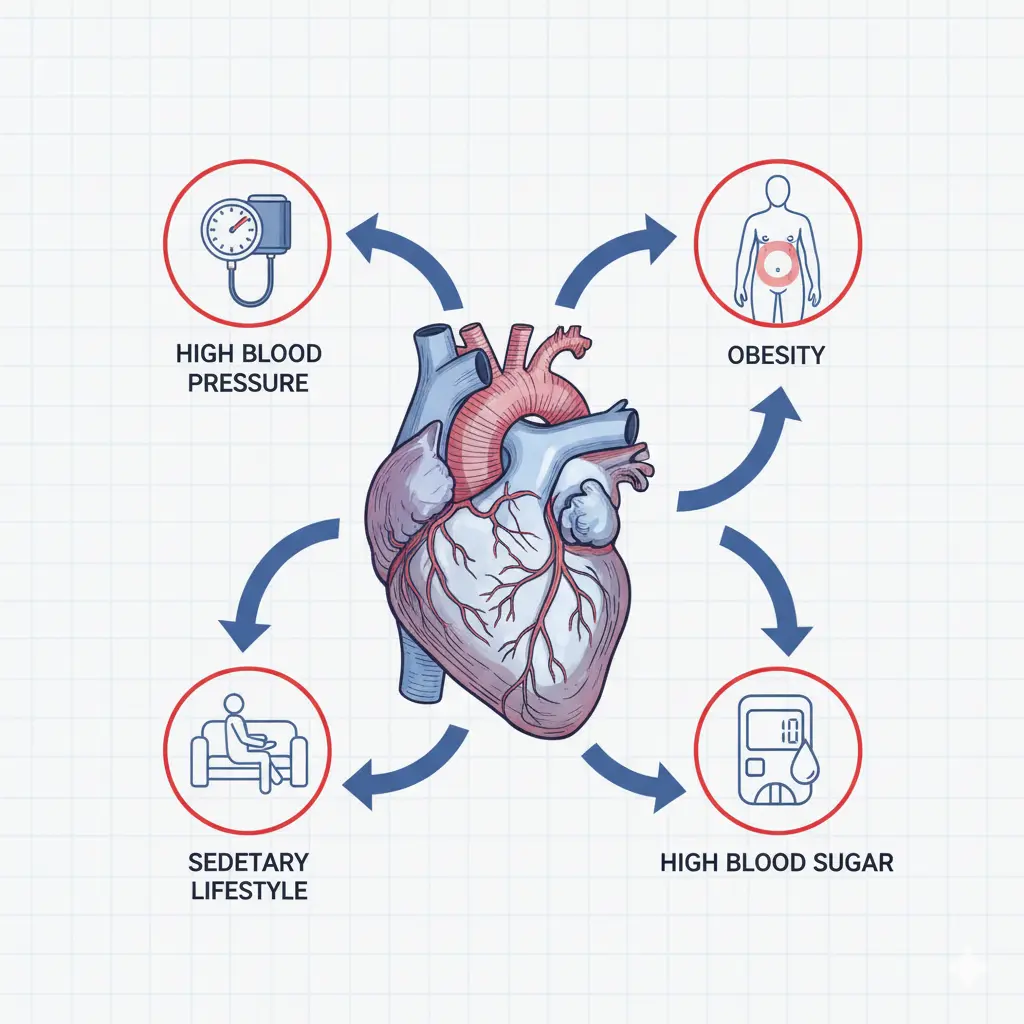
When delivered to the heart (often via intravenous infusion or direct injection), stem cells do not usually become new heart muscle in large numbers. Instead, they assist by:
- Secreting growth factors that support survival of existing cardiac cells
- Encouraging angiogenesis in ischemic regions to restore blood flow
- Suppressing excessive inflammation and fibrosis
- Improving microenvironment that helps surviving cells function better
These are mainly paracrine effects, meaning the benefits come from what the stem cells secrete, not necessarily from direct transformation into heart cells.
What the Evidence Shows
Stem cell therapy for heart disease remains largely experimental, but clinical trial data provide cautious optimism.
- A 2020 meta-analysis published in the European Heart Journal reviewed 21 randomized controlled trials on stem cell therapy for ischemic heart disease and heart failure. The study found modest but statistically significant improvements in left ventricular ejection fraction (LVEF), along with a trend toward reduced hospitalizations.
- Clinical studies in Asia, including intracoronary infusion of autologous mesenchymal stem cells (MSCs) combined with revascularization, have shown functional improvement in patients with ischemic cardiomyopathy.
- A 2021 cross-sectional survey identified 241 registered clinical trials of stem cell therapy for heart disease globally, with approximately 22% based in Asia, reflecting the region’s active participation in this field.
Treatment Workflow
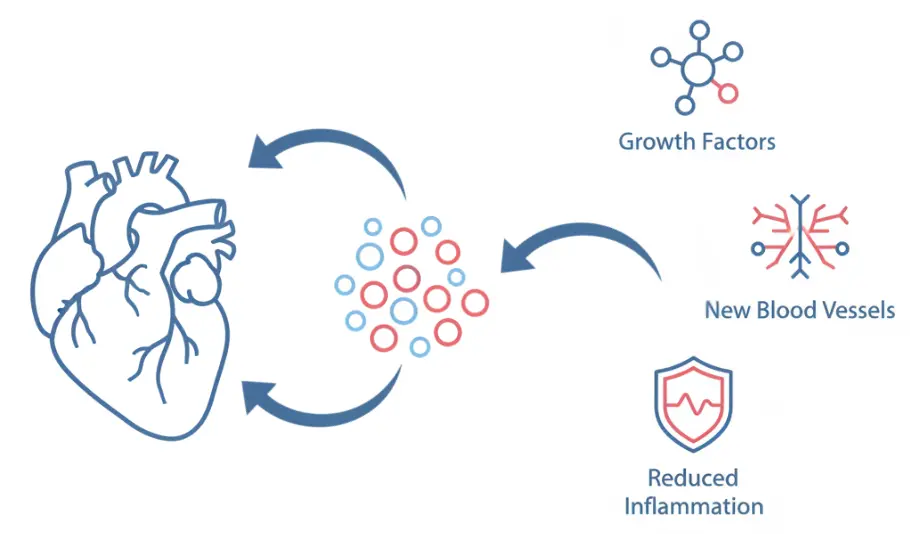
Pre-Treatment Evaluation
Patients typically undergo:
- Medical history and cardiac assessment
- Imaging (echocardiogram, MRI)
- Blood tests, ECG
- Screening for eligibility and risks
Cell Sourcing & Processing
Options include:
- Autologous MSCs: From patient’s own bone marrow or fat
- Allogeneic MSCs: Donor umbilical cord-derived, processed in GMP-certified labs
Cells are quality‑checked for sterility, viability, and potency before use.
Administration
- Intravenous infusion (most common)
- Intracoronary injection via catheter in some protocols
The procedure generally takes around 30-90 minutes in a controlled setting.
Post-Treatment Monitoring
- Continue standard cardiac medications
- Regular follow-up and imaging at 3-6 months
- Monitor for improvements and adverse events
Cost, Access, and Regulation
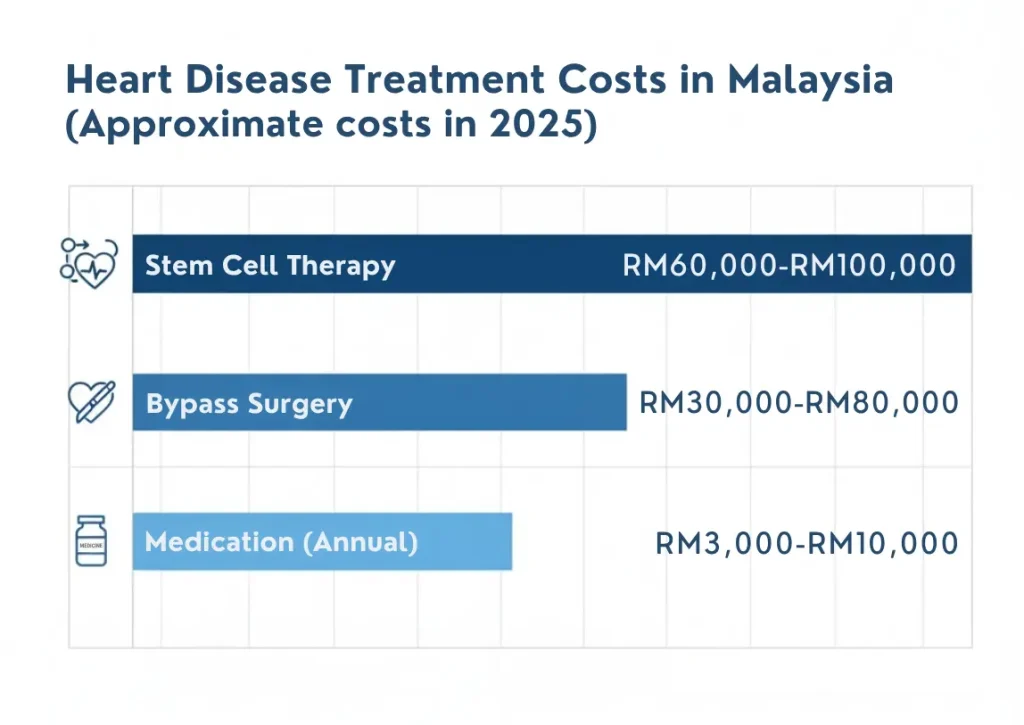
Cost in Malaysia (our primary treatment location): RM60,000-100,000 (approximately USD13,000-30,000).
Other Asian countries may have different pricing structures, typically ranging from USD 7,000-25,000 depending on the facility and protocol.
Insurance and Access
- Insurance typically does not cover stem cell therapy, as it’s considered experimental in most countries
- Some patients seek treatment in other Asian countries
- Private hospitals and specialized regenerative medicine centers are primary providers
- Public hospitals rarely offer stem cell therapy for heart disease as standard care
Regulatory Compliance
Treatment facilities should demonstrate:
- National health authority registration
- GMP-certified laboratory facilities
- Trained cardiovascular specialists
- Clear treatment protocols
- Comprehensive informed consent processes
Risks and Side Effects
Common Side Effects
Most patients tolerate MSC therapy well, but some may experience:
- Mild fever or fatigue (1-2 days post-infusion)
- Transient discomfort at injection site (if direct cardiac injection)
- Temporary increase in inflammatory markers
- Nausea or headache
Rare but Serious Risks
- Arrhythmias: Abnormal heart rhythms, particularly with direct injection methods (reported in <2% of cases)
- Immune reactions: If allogeneic cells are used (rare with MSCs due to low immunogenicity)
- Infection: Very rare when proper sterile protocols are followed (<0.5%)
- No therapeutic response: Approximately 30-40% of patients show minimal improvement or do not experience any noticeable effects after the treatment
Important Safety Considerations
- All procedures should be performed in facilities with cardiac monitoring capabilities
- Patients with certain arrhythmias may not be suitable candidates
- Long-term safety beyond 5 years is still being studied
- Any new chest pain, shortness of breath, or irregular heartbeat should be reported immediately
Benefits, Limitations, and Candidate Selection
Potential Benefits
- Slight improvements in ejection fraction or heart pump function
- Reduced symptoms and fewer hospital visits
- Enhanced quality of life in selected patients
Limitations
- Not a cure
- Response varies widely
- Benefits may emerge slowly (3-6 months)
- May require repeat therapy
- Long-term safety above 5 years remains under investigation
Who Might Be a Suitable Candidate?
- Patients with ischemic heart disease or moderate heart failure
- Those who are medically stable and already under cardiology care
- Individuals willing to accept the experimental nature and follow-up commitments
Not recommended for those with active infection, unstable disease, recent cancer, or severe organ failure.
Frequently Asked Questions (FAQ)
Q1: Is stem cell therapy safe for heart disease?
Clinical studies show low rates of serious adverse events when conducted in regulated settings.
Q2: How long until results appear?
Changes often appear after 3-6 months, and evolve over time.
Q3: Can it replace medications?
No. It is adjunctive, and patients must continue proven cardiac therapies.
Q4: Which Asian countries offer this therapy?
Major hubs include Singapore, South Korea, Japan, Thailand, China, India, and Malaysia.
Q5: How to choose a clinic?
Look for MOH registration, GMP lab accreditation, clear protocols, and multidisciplinary cardiology oversight.
Q6:What heart conditions are most suitable for stem cell therapy?
Early to moderate heart failure (ejection fraction 25-45%), ischemic cardiomyopathy, and post-myocardial infarction with residual damage are most commonly studied.
Q7: How many treatments are needed?
Most protocols involve 1-2 infusions. Some patients may benefit from repeat treatment after 12-24 months, but this is determined case-by-case.
Q8: Can it prevent future heart attacks?
No. Stem cell therapy aims to repair existing damage but does not prevent new cardiovascular events. Standard preventive care (medications, lifestyle) remains essential.
Conclusion
Stem cell therapy for heart disease in Asia represents a promising but still experimental frontier in cardiac care. It may benefit patients with residual heart damage who seek additional options beyond conventional treatments, but it is not a guaranteed cure.
Patients considering this option should consult cardiologists and stem cell specialists, verify facility credentials, and maintain realistic expectations.
For more information about stem cell therapy options in Asia, consult with qualified cardiovascular specialists or contact us.
ℹ Disclaimer
This article is for informational purposes only and does not constitute medical advice. Stem cell therapy for heart disease is an experimental treatment with ongoing research into its safety and effectiveness. Individual results vary significantly. Always consult licensed healthcare professionals for personalized medical advice and treatment decisions. Availability and regulations of stem cell therapy vary significantly by country.
Last Updated: October 2025